BOIL THAT WATER, SHE'S GONNA HAVE A BABY!
By Keith Souter, aka CLAY MORE
How many movies have you watched and heard those words? Quite a few, I imagine. Did you wonder exactly what the water was for? I mean, boiling water? Surely not to apply to the mother-to-be? But of course, you never find out because as soon as the water is brought in, the menfolk are rushed out and the expectant mother and her female neighbour, midwife or doctor are left to do their magic. Then you see the anxious father pacing up and down, acting clumsily or irrationally as he awaits that slapping noise, which was always followed by the cry of a newborn babe. Then the door opens and either a neatly wrapped baby is presented to the father or he is ushered in to see his wife with the baby ready for the proud father to see.
WARNING! THE REST OF THE ARTICLE IS GOING TO LOOK AT CHILDBIRTH, A SUBJECT THAT STILL MAY CASE FOLKS SOME ANXIETY. IF YOU ARE OF AN ANXIOUS DISPOSITION THEN READ NO FURTHER.
A natural birth
Nowadays most fathers attend antenatal classes and so they have a good idea of what is happening throughout the pregnancy. They know what to expect when labour begins, what they need to do, and a lot of fathers are present during the birth of their children. Some may been have delivered the baby themselves.
In the 19th century things were very different. Fathers didn't tend to have much to do with the pregnancy, apart from the obvious conception, of course. Most women received no antenatal care. When they went into labour they may have just gone somewhere on their own and given birth, or may have had a willing relative or neighbour that they could have help from. The father may have kept on working the land. A day or two after the birth she may have been back there helping him. Interestingly, this is still pretty much what happens in rural areas in the developing world.
Explanation of the birth mechanism from Fleetwood Churchill's 'On the Theory and Practice of Midwifery,' 1850.
So let's look at what happens
Pregnancy
This lasts 40 weeks, on average. A rule of thumb for calculating the expected date of delivery (EDD) is to take the first day of the last menstrual period (LMP) and add seven days, then subtract 3 months. This is working on the basis of conception occurring about two weeks before that, when ovulation, or the release of the egg from the ovary occurs.
During the first twenty weeks the baby is developing. During the second twenty weeks the baby's organs have all developed and it grows.
Another rule of thumb - the average mother will put on 28 pounds in pregnancy, 8 pounds only in the first 20 weeks, then a pound a week until term (ready to give birth).
Labour
There are three stages of pregnancy:
First stage - from the onset of contractions until the mouth of the womb (uterus) has opened up fully enough to allow for delivery. This can take 12-16 hours in a primiparous womb (first timer), but only 6-8 hours in a multiparous (a mother having had at least one previous pregnancy).
Second stage - the birth of the baby. This lasts 3-4 hours in a primiparous women, but may be very fast in a multip.
Third stage - the delivery of the placenta, or afterbirth. It usually comes away within half an hour of the birth of the baby.
After the baby is born the cord is ligated and separated. This is done a few inches from the umbilicus. This umbilical stump will gradually shrivel and separate after a few days. It used to be advised to cut quickly, but modern research suggests that waiting until the placenta has delivered gives a premature baby more blood and more stem cells, all of which is better for them.
Complications
While the majority of pregnancies do go through to an uncomplicated labour and birth of a child, yet there are still a considerable number that have complications. There can be problems with the baby as the result of failure to develop one organ or another. The result can be miscarriage, when nature ends the pregnancy or stillbirth of a dead baby, or birth of a baby with a congenital malformation.
There can be problems with the pregnancy itself; for example, difficulties with the mother's blood pressure, which can lead to kidney failure, convulsions and even death. Nowadays we are familiar with pre-eclampsia, toxaemia of pregnancy and the various related problems, but back in the mid-nineteenth century there was no conception about blood pressure, so no way of helping.
Then there can be problems about the position of the placenta. If it is too low, which we call
placenta praevia, then this can produce hemorrhage either before labour or during labour if it detaches from the uterine wall.
The cord can prolapse during labour. That means it can come out before the baby and the baby's own head can therefore obstruct its own blood supply.
And there can be problems about going over term, or just not progressing during the labour. These are things that we can do a lot about nowadays, but back then there were a limited number of drugs and herbs that could be used.
[I'll be looking at herbs and drugs in a later blog.]
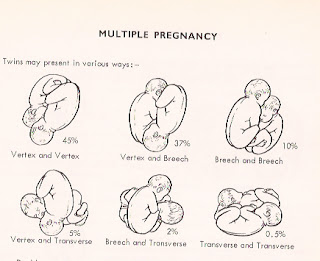
Multiple births
Twin and triple pregnancies occurred and would challenge whoever was assisting the mother. These are more likely to be difficult labours and there is a lot of potential for things to go wrong with both babies. You may think that if a baby is born quickly then all will be well. Not necessarily. If a baby is born too quickly there can hemorrhage into the baby's brain.
Twins presentation in The Rose Garden, a 1513 publication for midwives
And of course, there can be problems from the twins' positions. Caesarian sections would not have been a ready option and a good midwife or doctor would be essential.
Good old Doc Adams was adept at delivering babies and looking after the newborn. Indeed, in
The Baker's Dozen, from Gunsmoke's season 13, in 1967, he is involved in the aftercare of triplets who were born to a woman who arrived in Dodge City on a stage that had just been robbed. The mother sadly dies in the process, and it transpires that the father was a stage robber who has been killed. Doc looks after the triplets and is determined that they should be kept together and not sent to the State orphanage.
Malpresentations
When we assess a mother's abdomen we talk about the presentation. That means the anatomical part of the baby that is leading and which is likely to be born first. There are whole number of ways that we refer to them - cephalic, meaning the head first. This is the one we always want to find. There are variations, of course, so you can have vertex (top of head), sinciput (forehead), face, chin, occiput (back of head) and others.
Other presentations are called malpresentations. Thus a foot, a shoulder, a hand or a bottom (breech) all present difficulties for the doctor or midwife. Indeed, nowadays with good antenatal care you aim to know precisely how a baby is lying well in advance of the due date and plans can be made. This may well be a planned Caesarian Section. Back in the 19th century there were no scans, everything had to be worked out through clinical acumen alone and the use of a simple foetal stethoscope.
The author's foetal stethoscope - which is more or less obsolete today, since most doctors have an ultrasound gadget
A breech presentation occurs in about one in every 40 cases. It is a common position early on in about a quarter of pregnancies, but a fair number will turn round before the critical 36 weeks stage. In the 19th century the first inkling of this would probably be at term, when the woman was going into labour. Again, nowadays we would aim to know well ahead and plans would be made.
External cephalic version is the name of the technique used in trying to turn a baby from the outside. It would be done from 32 weeks to 35.
External Cephalic Version - an attempt to gently turn the baby from breech to cephalic presentation in advance of term
The instruments
Most frontier doctors would carry obstetric instruments with them. That is they would have obstetric forceps to help to deliver the baby's head when it is is in the vagina and effect delivery by traction without causing injury.
There are several types, but the common features are the two curves. They have a cephalic curve to be applied to the baby's head, and they are have a pelvic curve to fit the pelvic curve of the birth canal.
Not only would a doctor carry forceps, but he would have instruments to perform an episiotomy, an incision needed to allow room for the forceps and often also to give a baby enough room to get out. He would also have to have sutures and instruments to repair the episiotomy.
Yet sadly, he would also have to carry other instruments in case things had gone wrong and the baby had died. I think that is as far as I need explain, but if anyone would wish for further information, then I can be contacted off-line.
Sepsis - the great killer
At this point we really have to talk about maternal mortality. Here I am going to talk about the situation in the UK, since I am more familiar with it and have figures. I believe that the points are still germane when applied to the USA and the frontier.
At the beginning of the 19th century pregnancy and childbirth carried significant risks for the health of a woman. One in 200 women died in childbirth. In part this was to do with complications of being poor, of not having enough money for food. Rickets, due to vitamin D deficiency caused skeletal problems and pelvic distortions, so labour could be difficult and become obstructed with catastrophic results for mother and child.
Yet the maternal mortality in hospitals was actually greater! That is right, you had a higher risk if you went into hospital for treatment. They did not realise it, but the problem was
puerperal fever - which they recognised - but they still did not understand the problem of sepsis.
In fact, a Scottish physician, Dr Alexander Gordon, working in Aberdeen had made the link at the end of the 18th century when he deduced that there was a connection between puerperal fever and erysipelas (an infection later found to be due to Streptococcus). He wrote a treatise about it, but it had no impact. He drew a significant conclusion and stated that he believed that somehow doctors and midwives spread the problem. Yet along with his fellow physicians he advocated that the treatment should be venesection or bleeding.
Oliver Wendell Holmes (1809-1894), a doctor, poet and writer, sometime dean of Harvard Medical School, also made the connection and suggested that doctors in particular were the problem. He went so far in a paper of 1843 to suggest that doctors who conducted autopsies should not also practice obstetrics.
Professor Oliver Wendell Homes
Yet history proclaims Ignatz Semmelweis (1818-1867) as the man who made the breakthrough. He published a treatise in Budapest in 1861, entitled ‘The Cause, Concept and Prophylaxis of
Puerperal Fever.’ It was based on work he conducted in the 1840s. He suggested that women who died from puerperal fever
(childbearing fever) had been contaminated by doctors who had not washed their
hands between attending morning autopsies and going to the labour wards. He was castigated by his fellow practitioners for daring to suggest that they should wash their hands, without any 'scientific evidence' as to why. It was said that he was not saying anything new, it was just the same thing that Holmes had been saying.
He actually suffered a nervous breakdown and was committed to an asylum in Vienna, where he died a fortnight after his committal, after having been beaten by guards.
Dr Ignatz Semmelweis
Semmelweis was vindicated after his death when Lister started using carbolic acid sprays and advocated strict hygiene. And most importantly, Louis Pasteur proved the germ theory of infection.
Another reason for morbidity in hospitals was the tendency to make women 'lie-in,' or stay in bed for a couple of weeks after birth. This is not a good idea, since the risk of blood clotting is increased. Yet again, the women on the frontier who needed to get going to fix the corral or feed the animals, possibly fared better.
Caesarian sections
These are operations performed to remove the child from the mother's womb through an incision in the abdomen. They first one to be done in which the mother survived was in Ireland in 1738. The first in England was performed by Dr James Barlow in 1797 and the first in the USA was by Dr John Richmond in 1827. These were all done without anaesthetic and so when anaesthesia became generally used, together with aseptic surgical techniques, Caesarian Sections became viable operations.
In the 1880s the classical Caesarian Section method was developed, which involves a longitudinal incision in the upper uterine segment. That is, in the upper part of the womb. These do not heal well, so they were replaced in 1906 by the lower segment Caesarian section. This is the method favoured today, although under certain situations the classical may be performed.
So what about that boiled water?
Well, it would be useful. Not only to sterilise as best one could the instruments, but also to use to make warm(not booing) compresses to place over the perineum prior to labour. This would tend to soften the tissues, which get stretched, of course, and lessen pain and reduce tearing of the tissues.
And of course, it would be for washing hands and swabbing everything down afterwards. On the point of washing hands, it should be noted that the frontier doctor's hands would probably have a greater need of being washed than would a midwife. Quite simply, the midwife would not be handling purulent matter, operating on diseased tissue or conducting autopsies. Nor would she have been exposed to coughs and sneezes to the same extent as the doctor.
And that slap on the back?
Well, we don't do that any more either. Doctors and midwives used to do it to stimulate the baby, in the belief that you needed it to help it to breathe and to cry to clear all those secretions out of nose and mouth. Now we just suck it out with a tube and if needed, give controlled oxygen.
A couple of final points about cutting the cord
This is really if you ever find yourself having to deliver a baby. Don't go searching for a scissors of anything else to cut that cord. nature generally does a good job. Don't cut it, or tie it off, just call the emergency services and let them clamp it off for you. As noted above, a slight delay is no bad thing, and may be quite beneficial to the baby.
Lastly, any cutting of a cord has to be done with a clean instrument. I say this from experience of many moons ago, when I was working in a fever hospital in India. There was a whole ward devoted to cases of neonatal tetanus. Almost all of them had been due to injudicious severing of the cord with any sharp object hat was at hand- knives, scissors, sickles!
Tetanus or Lockjaw is a horrid condition - which I'll be getting round to at some stage.
__________________________________________________________________________
Hell on the Prairie, the sixth Wolf Creek book features Keith (Clay More's) character Dr Logan Munro, the town doctor in THE OATH, a story about a spectre from his past. Logan has been in Books 1, 4 and 6, and is due to appear in books 8 & 9.
And his other new character, Doc Marcus Quigley, dentist, gambler and occasional bounty hunter continues in his quest to bring a murderer to justice, in AMBUSH AT DEAD MAN'S RAVINE, the fourth in his monthly ebook short stories THE ADVENTURES OF DOCTOR MARCUS QUIGLEY published by High Noon Press.
Vol 5 THE SHOOTER should be out soon.




.jpg)














.jpg)